Villanova Nursing and Philadelphia College of Osteopathic Medicine Answer National Imperatives and Collaborate for Interprofessional Education
Mock Code Simulation Advances Earlier Nursing Research to Improve Safety and Outcomes During Transitional Care for Patients with Parkinson’s Disease
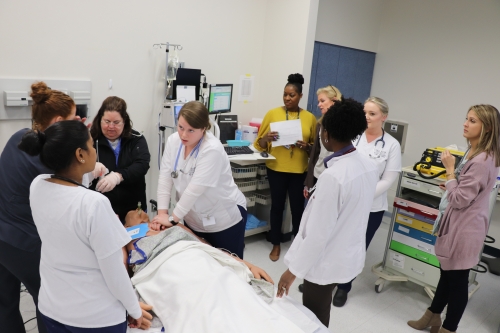
Patient safety and interprofessional coordination and communication is being enhanced as Philadelphia area nursing, medicine and psychology students come together throughout the year in mock code simulations to drive cross-discipline understanding and ultimately improve patient outcomes. Creating high functioning teams that can collaborate and communicate aligns with national movements to improve patient safety and provide quality care at reduced costs. The initiative stems from an Institute of Medicine (now the National Academy of Sciences, Engineering and Medicine) report of the last decade.
Since spring 2019, bachelor-level nursing students and doctoral-level nurse anesthesia students from Villanova University M. Louise Fitzpatrick College of Nursing, and doctoral-level students in osteopathic medicine and psychology from Philadelphia College of Osteopathic Medicine (PCOM), have joined forces in their education to enhance patient care through a copyrighted mock code simulation- one in which the students practice their respective roles during a cardiopulmonary arrest as well as in a code team debrief in a simulated environment. The core issue in the simulation scenario is missed medication during a transition in care.
“While technology and medication make resuscitation possible, it is the nexus of highly educated health care professionals and their effective communication and coordinated action that count as much as the seconds that tick by. That human interaction and intervention is critical to saving lives,” notes Donna S. Havens, PhD, RN, FAAN, Connelly Endowed Dean. “We are proud of the model created by our Parkinson’s disease (PD) research team here which weaves safety in care transitions throughout and is building much needed science; we are equally proud of our collaboration with PCOM which has further strengthened students’ experiences.”
For patients hospitalized with PD, instances of missed, omitted or delayed medication occur frequently, including during transitions in care. These medication errors increase length of stay and can also cause significant co-morbidity, including falls, aspiration and death. To prevent such errors, Diane M. Ellis, MSN, RN, CCRN, clinical assistant professor at the Fitzpatrick College of Nursing - and an expert in the care of people with PD - designed an evolving body of simulation research, assisted by faculty, simulation staff and research seminar students. It began with nursing students understanding medication safety for PD patients in care transitions, then incorporated nurse anesthesia students as part of the simulated code team.
"Nurse anesthesia students encounter many high-risk patients during their clinical education. This experience has allowed them the opportunity to utilize and share their educational background and experiences, while collaborating with other health care providers in the care of a vulnerable high-risk patient" said Carlene McLaughlin, PhD, CRNA, co-investigator and nurse anesthesia program faculty member.
In Spring 2019, this research entered its third phase, which includes an interprofessional mock code simulation. Its goals are to increase awareness and educate health care professionals regarding the harm that PD medication errors can cause during a care transition and to improve comfort with interprofessional collaboration and communication.
“PCOM was more than happy to collaborate with Villanova and its nursing students on this important initiative addressing a high-risk population, while also learning how to work together to put the patient’s needs first,” said Michael Becker, DO, MS, assistant dean of clerkship education. “This person-centric thinking has been a main tenet of the osteopathic profession since its founding.”
"Clinical psychologists are broadening their roles to be included as health service providers,” said Stephanie Felgoise, PhD, associate dean, academic integration, and Clinical PsyD program director. That program, she says has “traditionally focused on holistic care alongside of the osteopathic medical school, and this new initiative further enhances the IPE at PCOM by having students learning from, with, and about nurses' education.
The faculty, students, and staff at Villanova’s College of Nursing have become valued colleagues and friends throughout this experience,” she added.
This study, being conducted in the Fitzpatrick College of Nursing’s Simulation and Learning Resource Center, holds great potential for dissemination among health-care professionals to improve quality, safety, education, communication and collaboration specific to Parkinson’s patients during care transition. A novice nurse’s top concern is what to do in a code situation, according to the literature. Mock code simulations have been shown to increase nurses’ confidence when a crisis does occur.
Observes Ellis, “It was our aim to create innovative case studies for simulation to improve care for this vulnerable, ‘high risk, low volume’ population by increasing awareness of the impact of errors with patients’ PD medications. When completed next year, this third study combined with the previous two studies will have reached approximately 1,000 health-care professionals from various disciplines. This is just the start.”
